66yr old male with fever 3 days and DM 2 20 years
June 07, 2023
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
Case report
A 66 year old daily labourer by occupation presented with chief complaints of high grade fever since 3 days and generalized weakness since 1 day.
Patient was apparently asymptomatic 3 days back when he went to some function and then the next day he developed high grade fever insidious in onset that is associated with chills and rigors, intermittent type relived with medication without any diurnal variation.
Then the patient went to a local doctor where he was prescribed with some medication and his fever got relieved on taking medication.
Then he developed generalized weakness which is insidious in onset due to which he was unable to perform routine activity and was brought to our hospital.
H/O giddiness present since yesterday, H/O fall present (two times), H/O Loss of conciousness for 5 min
No H/O SOB, chest pain, palpitations
No H/O cough, cold, vomiting.
Daily routine
Patient wakes up at 6 am then gets freshened up, takes tea at 7 am eats breakfast at 8 am and then goes to work as a daily labourer and then comes back home at 1 pm takes lunch then sleeps for 2 hours then takes tea at 6 pm and eats dinner at 8 30 pm and goes to sleep by 9 30 pm.
Past history
K/c/o DM 2 since 20 years and is on regular medication since then.
When patient went to a local doctor his blood pressure was high and was told to take antihypertensive medication since 2 days.
Not a k/c/o asthma, epilepsy, CAD, CVA, thyroid disorders.
Patient is a known case of FILARIASIS of left lower limb and scrotum.
Personal history
He takes mixed diet with normal appetite and has regular bowel and bladder movements.
He takes alcohol daily since 1 year.
Family history
No significant family history
General examination
Pallor is present.
No features indicating the presence of icterus, cyanosis, clubbing, edema lymphadenopathy.
SYSTEMIC EXAMINATION
ABDOMINAL EXAMINATION
INSPECTION
No distention,No scars
Umbilicus - Inverted
Equal symmetrical movements in all the quadrants with respiration.
No visible pulsation,peristalsis, dilated veins and localized swellings.
PALPATION
No local rise of temperature, Abdomen is soft with no tenderness.
No spleenomegaly, hepatomegaly.
PERCUSSION
Liver span is 12cm, No hepatomegaly
Fluid thrill and shifting dullness absent.
No puddle sign.
AUSCULTATION
Bowel sounds present.
CVS- S1 and S2 heart sounds heard.
RS- Bilateral air entry is present, normal vesicular breath sounds heard.
CNS EXAMINATION
Right Handed person, uneducated
HIGHER MENTAL FUNCTIONS:
Conscious, oriented to time place and person.
speech : muffled, unclear
Behavior : normal
Memory : Intact.
Intelligence : Normal
No hallucinations or delusions.
CRANIAL NERVE EXAMINATION:
Intact
MOTOR EXAMINATION:
Right Left
BULK UL Normal Normal
LL Normal Normal
TONE UL Normal Normal
LL Normal Normal
POWER UL 5/5 5/5 LL 5/5 hypotonic?
REFLEXES
Right Left
BICEPS ++. ++
TRICEPS +++ ++
SUPINATOR + +
KNEE +++ ++
ANKLE - -
PLANTAR flexor flexor
SENSORY EXAMINATION: intact
PROVISIONAL DIAGNOSIS
VIRAL PYREXIA
DM 2 SINCE 20 YRS
INVESTIGATIONS
ECG
Chest xray
SEROLOGY
HBsAG- Positive
HIV, HCV- Negative
USG Abdomen
Grade 1 RPD changes in Left kidney
Left simple renal cortical cyst
CBP 6/6/23
Lft
6/6/23
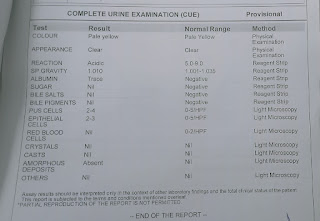
Cue
FBS- 70mg/dl
PLBS-167mg/dl
Blood urea-37mg/dl
Serum creatinine- 1.8mg/dl
Serum electrolytes-6/6/23
Treatment
Inj.Monocef 1gm IV/BD
Tab.Dolo 650mg PO/TID
Inj.Neomol 1gm IV/SOS if temp more than 101 F
Soap notes
8/6/2023
AMC BED 5 - 66M
S:
Fever spikes present
O:
Patient is drowsy
BP: 130/80 mmHg
PR: 94 bpm
RR: 24 cpm.
Spo2: 98%
CVS: S1 s2 heard , no murmurs RS: B/L air entry present No added sounds
CNS: No FND
A:
Viral pyrexia ?Typhoid fever
K/c/o DM 2 since 20 years
P:
1)Inj.Monocef 1gm/IV/Bd (D2)
2)IV fluids NS@100ml/hr
3)Inj.Neomol 1gm/IV/SOS
4)Inj.HAI according to GRBS >200mg/dl
5)Tab.Dolo 650mg/PO/TID
Soap notes
9/6/23
AMC bed 5
S:
Fever spikes present
O:
Pt is conscious, coherent and cooperative
BP - 130/80 mmHg
PR- 80 bpm
RR - 18 cpm
Temp - 100 F
GRBS - 167 mg/dl
SpO2 - 99% @RA
CVS - S1 S2 heard , no murmurs
RS - BAE+ no added sounds
P/A - soft and non tender
CNS - no FND
A:
PYREXIA ? TYPHOID FEVER K/C/O DM II SINCE 20 YEARS WITH HBsAg +
P:
INJ. MONOCEF 1 G IV/BD
IV FLUIDS NS @ 100 ml/hr
INJ NEOMOL 1 G IV/SOS
TAB DOLO 650 MG PO/TID
INJ HAI ACCORDING TO GRBS
Soap notes
10/6/23
AMC bed 5
S:
Fever spikes present yesterday
Did not pass stools since 2 days
O:
Pt is drowsy
BP - 140/60 mmHg
PR- 97 bpm
RR - 16 cpm
Temp - 100 F
GRBS - 235/dl
SpO2 - 98% @RA
CVS - S1 S2 heard , no murmurs
RS - BAE+ no added sounds
P/A - soft and non tender
CNS - no FND
A:
PYREXIA SECONDARY TO ? TYPHOID FEVER
? MENINGITIS
K/C/O DM II SINCE 20 YEARS WITH HBsAg +
P:
(D5) INJ. MONOCEF 1 G IV/BD
(D4) INJ DOXYCYCLINE 200 MG IV/BD
IV FLUIDS NS @ 100 ml/hr
INJ NEOMOL 1 G IV/SOS
TAB DOLO 650 MG PO/TID
INJ HAI ACCORDING TO GRBS









.jpg)







Comments
Post a Comment