This is an online E log book to discuss our patient's
de-identified health data shared after taking her guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
MUSKAAN GOYAL , 8TH SEM,
ROLL. NO: 92
MAY 18,2021
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
(Contains information collated from Dr.CHANDANA PG and from the patient)
CASE DISCUSSION:
A 78 yr old male patient, resident of of kattangur and shepherd by occupation came to the Opd on 14 /5/2021 with chief complaints of :
SHORTNESS OF BREATH ,SINCE 20 DAYS
CHEST PAIN ,SINCE 20 DAYS
B/L PEDAL EDEMA , SINCE 4 DAYS
FACIAL PUFFINESS , SINCE 4 DAYS
HISTORY OF ILLNESS :
Pt. who is chronic smoker and alcoholic ( 90ml of toddy/whisky) since 30 years was apparently asymptomatic 1 month ago ,then he suddenly developed
SOB -grade 3 . He then went to a local RMP and took injection (unknown) and following the injection sob subsided in one day. After 10 days he again developed SOB grade 3 which progressed to grade 4 , 2 days back. H/O orthopnea present . NO H/O PND.
SOB was associated with diffuse chest pain ,pricking in nature since 20 days.
NO H/O fever, cold, cough, palpitations, decreased urine output.
K/C/O HTN since 1yr ( using TAB. TELMA 40MG)
K/C/O DM since yr( using TAB.GLINIPERIDE 1 MG)
ON 1/5/2021:
Pt. went to local hospital in view of the chest pain , where they did routine investigations and told he has heart problem and raised creatinine. TROP 1 was negative at this time .
2D ECHO:
normal lv function with mild pericardial effusion.
ECG :
diffuse 1mm ST elevation
first degree AV block
? acute pericarditis
BLOOD FINDING:
1, Hb- 8mg/dl
2,tlc- 13.700
3, platelets- 3.8lakhs
4, serum creatinine - 1.3mg/dl
5, CRP- 11.3
ON 4/5/2021:
As the pt. had no improvement in symptoms, pt. was advised as ECG and 2D ECHO again .
drugs prescribed : TAB. LASIX
TAB. CLOPIDOGREL.
atrial premature complexes present
ON 5/5/21 :
The pt. was advised a ECG.
ECG :
low voltage complexes present
ON 9/5/2021:
pt. has no much improvement in symptoms and so was prescribed few drugs and referred to a higher Centre.
PRESCRIPTION
ON 10/5/21:
Pt. went to another hospital and got an echo but did not consult the cardiologist.
serum creatinine was 2.14 mg/dl.
trop i negative at this point.
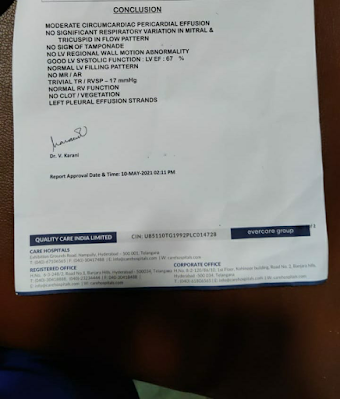
2D ECHO
echo showed normal lv function with mild pericardial effusion
ON 14/5/2021:
Pt. presented to KIMS due to increase in SOB with other associated chief complaints even after using the previous prescribed medication by a doctor in local hospital.
ON EXAMINATION AT THE TIME OF PRESENTATION:
GENERAL EXAMINATION:
pt. was C/C/C
well oriented to time , place and person.
pallor + ( present)
NO icterus, clubbing, cyanosis, lymphadenopathy.
B/L pedal edema + ( pitting type)
VITALS:
temperature - afebrile
PR- 90 bpm , REGULAR
RR- 32 cycles/min
SPO2- 98% on RA
GRBS- 174mg/dl
BILATERAL PEDAL EDEMA( PITTING TYPE)
SYSTEMIC EXAMINATION:
CVS-
elevated JVP
muffled s1 s2
RESPIRATORY SYSTEM
B/L air entry present
dyspnea - present
wheeze - absent
ABDOMINAL EXAMINATION
soft and non tender
bowel sounds can be heard
INVESTIGATIONS:
ECG , 2D ECHO , USG ABDOMEN , CHEST X-RAY , BLOOD REPORTS
X- RAY CHEST
first degree av block present
no ST elevation.
normal axis and no LVH
USG ABDOMEN
BLOOD REPORTS
2D ECHO WITH VIDEO ABOVE
moderate pericardial effusion
normal sized chambers and good lv function
IVC dilated and non collapsible
ON 15/5/2021:
Pt. developed hypotension early in the morning , therefore was started on NOR ADRENALINE infusion AND INOTROPES.
To keep a check if Pt. is having cardiac tamponade , review of ECHO is being done .
we have noticed a swelling on lateral side of neck, assuming it be to lymph node enlargement due to TB . Therefore a USG NECK AND SPUTUM FOR AFB was done.
2D ECHO ( REVIEWED)
no cardiac tamponade found
USG NECK :
swelling was just a superficial soft swelling and not a lymph node
SWELLING ON LATERAL ASPECT OF NECK
SWELLING ON LATERAL ASPECT OF NECK
SPUTUM FOR AFB WAS NEGATIVE ( therefore ruling TB)
ON 17/5/2021:
Pt.is still hypotensive , therefore NOR ADRENALINE infusion is being continued. but there seems no much improvement with it.
to keep a check on cardia tamponade, review echo was done.
2D ECHO (REVIEWED)
no cardia tamponade seen
ON 18/ 5/2021:
Pt. is still hypotensive with BP of 80/60mmhg.
As there is no much improvement in hypotension even after NOR ADRENALINE infusion since past three days , the drug has been stopped today morning.
As the patient is anemic with hemoglobin levels of 8mg/dl , planning to send blood sample for serum ferritin .
HRCT is being planned to look for any mediastinal lymph nodes and to rule out any lung malignancies.
ON 19/5/2021:
Patients blood pressure is 90/60mmhg without nor adrenaline. He is presently stable without any additional drugs apart from medication he is using with HTN and DM .
Oxygen saturation is normal in RA.
Today planning for a USG guided pleural tap.
HRCT REPORTS FOR THE PATIENT HAS COME.
HRCT REPORTS:
- NO mediastinal lymphadenopathy
- moderate pericardial effusion
- bilateral moderate pleural effusion.
XRAY CHEST :
showing minimal effusion on left side
ON 20/5/2021:
On USG , only a small pocket of 1cm effusion which was obliterating with inspiration was found . As there is risk for lung injury pleural tap has been avoided and is planned for discharge today.
Pt. has been managed conservatively and his complaints of SOB, chest pain subsided and B/L pedal edema has reduced at the time of discharge.
DIAGNOSIS :
Acute pericarditis with moderate pericardial effusion secondary to ? post viral? post MI
( resolving : 2.07cms effusion at the time of admission -1.4mm at the time of discharge)
DM type 2 (since 1month)
ADVICE AT THE TIME OF DISCHARGE:
TAB. Glimepiride 1mg PO OD
TAB. Lasix 20mg PO BD
TAB. Ultracet half tab SOS
TAB. MVT PO OD
fluid restriction (<1.5lt/day).























Comments
Post a Comment