35yr old female know case of polio comes with fever and cough
This is an online E log book to discuss our patient's
de-identified health data shared after taking her guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
MUSKAAN GOYAL ,
ROLL NO. 92
October 18, 2021
A 35yr old female presented to the causality at 6 O clock on 17 /10/2021 with chief compliants of
FEVER SINCE 4 DAYS
COUGH SINCE 4 DAYS
VOMITING SINCE MORNING
HISTORY :
35year old unmarried female born out of non consanguineous marriage first in birth order .she studied till 1st standard . At age of 6 , one day she suddenly developed fever high grade nd associated left upper limb and lower limb weakness and she was diagnosed to have polio. She was taken to thirupati for some surgery which was advised by one of her neighbour who aslo suffered from polio. She underwent surgery in thirupati which was unsuccessful
She was on oral medication for 2yrs , over time she regained power in Lt.UL and LL . She does her own household chores and takes care of herself nd her family members .
Since then patient had no major illness.
She has now been experiencing fever since 4 days which is sudden in onset ,high grade nd continuos nd doesn't relief on medication and there is no diurnal variations .
Fever is associated with cough which is non productive.
Pt also had 3 episodes of vomiting which was non bilious , non blood stained and non projectile since morning .vomiting was mainly after a episode of cough.
PAST HISTORY:
No similar complaint in past.
No h/o DM , HTN , CAD , EPILEPSY , TB
FAMILY HISTORY :
No significant family history.
PERSONAL HISTORY:
Diet : mixed
Appetite : decreased since she was having fever
Sleep : disturbed due to cough
Bowel and bladder : regular
No know drug and food allergy
No addictions
GENERAL EXAMINATION:
Pt was concious , coherent and we'll Oriented to time , place and person
Moderately built and we'll nourished
No pallor , icterus , cyanosis , clubbing , lymphadenopathy , edema
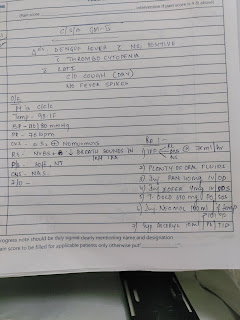
Vitals at the time of admission:
Temp- 98.1F
PR- 95BPM
RR- 20/MIN
BP- 100/80MMHG
SPO2- 99% at room air
GRBS - 138mg%
SYSTEMIC EXAMINATION :
Respiratory:
Bilateral inspiratory crepts in all lung fields.
Cvs:
S1 S2 heard
No added murmures
Per abdomen:
Soft and non tender
Bowel sounds heard
CNS:
Higher functions intact
Motor system :
Tone increased in upper left limb and lower limb .
Power :. Upperlimb. Lowerlimb
Rt 5 5
Lt 4 4
Reflexes
Right Left
B 2+ -
T 2+ -
S 2+ -
K 3+ 3+
A + +
P Flexion bilaterally
INVESTIGATIONS :
Hemogram , RFT , LFT , NSI ANTIGEN , SEROLOGY , CHEST XRAY , ECG
















Comments
Post a Comment