This is an online E logbook to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from an available global online community of experts to solve those patients clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box are welcome.
MUSKAAN GOYAL
ROLL NO. 92, 8TH SEM
MAY 26,2021
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
(Contains information collated from Dr.CHANDANA PG and from the patient)
CASE DISCUSSION:
A 61 yr female pt. , farmer by occupation , resident of chandanpet presented to the Opd on 25/5/2021 with chief complaints of
FEVER SINCE 5 DAYS
VOMITING SINCE 3 DAYS
COUGH SINCE 2 DAYS
SHORTNESS OF BREATH SINCE AFTERNOON
HISTORY OF PRESENT ILLNESS:
Pt. was apparently asymptomatic 5 days back and the she suddenly developed ,
fever which was sudden in onset , intermittent in nature , on and off with chills and rigor and relieved on medication . Pt. took self prescribed medication for fever . ( TAB. DOLO ).
fever is associated with body pains.
vomiting since 3 days 3episode per day which is mostly after intake of solid food , content being the food taken . not associated with pain abdomen and loose stools.
cough since 2 days which was sudden in onset , non productive , and no aggravating and relieving factors.
SOB since afternoon which is grade 3 . NO H/O orthopnea and PND. did not take any oxygen inhalation
NO H/O pedal edema , facial puffiness and burning micturition.
HISTORY OF PAST ILLNESS:
Pt. developed fever 5 days back , for which she started taking TAB . DOLO ( self prescribed) for 2 days .
After that she has unbearable body pains following which she got a covid-19 test done which came out positive ,following that she took TAB. DOLO , TAB. DOXYCYCLIN and TAB. LIMCEE ( all self prescribed ).
she then developed SOB for which they consulted a doctor near by who advised for a HRCT scan which showed lung damage .
Following this , the pt. was brought to KIMS yesterday night.( 25/5/2021).
No H/O DM , HTN , epilepsy , CAD , CNA , TB , CKD .
FAMILY HISTORY :
Patient's husband has also been tested covid-19 positive and is on medication and in home isolation.
PERSONAL HISTORY:
diet - mixed
appetite- reduced since 3 days
sleep- disturbed due to body pains since 3 days
bowel and bladder - regular
addictions- no addictions
GENERAL EXAMINATION:
Pt. is C/C/C
heavily built and obese
NO pallor , cyanosis , icterus , clubbing , lymph adenopathy , edema
obese with central obesity.
VITALS ON THE TIME OF ADMISSION:
temperature - afebrile
PR- 120 beats per min
RR-28 cycles / min
BP - not recorded
SPO2 - 75% at ROOM AIR
SYSTEMIC EXAMINATION:
CVS:
S1 S2 heard . no murmurs
RESPIRATORY SYSTEM :
B/L coarse crepts present
dyspnea present
centrally place trachea
no wheeze
CNS :
no abnormal defects
ABDOMEN:
soft and non tenser
bowel sounds normal.
INVESTIGATIONS:
pt. has got HRCT done in other diagnostic center before coming to the hospital.
COURSE IN HOSPITAL :
25/ 5/2021:( day of admission)
Pt. was examined and started on medication and oxygen inhalation to maintain spo2 above 92%
INVESTIGATION : blood reports and ECG advised.
26/5/2021:( day 5 of illness)
Pt. complains of epigastric pain after breakfast.
VITALS :
temperature: afebrile
BP: 120/90MMHG
RR: 21 cycles per min
PR- 76 beats per min
spo2 - 91 on 15lt of oxygen .
grbs- 149mg/dl
INVESTIGATION : advised for serum ferritin , LDH , repeat ECG.
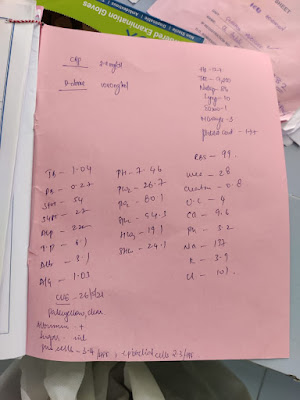
BLOOD REPORTS AND ECG REPORTS:
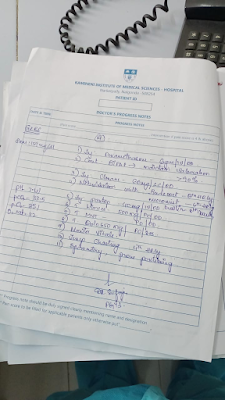
TREATMENT BEING GIVEN.
27/5/2012: ( day 6 of illness)
CT SEVERITY SCORE - 15/25( according to 25/5/21)
CORADS-5
ON BIPAP.
O/E -Pt. is C/C/C
vitals at 8:00 am :
temperature : afebrile
PR: 102bpm
BP: 110/70mmhg
GRBS: 159mg/dl
spo2 : 83 % on continuous BIPAP
CVS : s1s2 +
R/S : BAE +
P/A :
soft and non tender with no organomegaly.CNS- HMF intact
NO pedal edema , jaundice .
INVESTIGATION ADVISED TODAY IS 2D ECHO.
TREATMENT TODAY:
28/5/2021:(day 7 of illness)
CT SCORE -15/25
CORADS - 5
8 am:
O/E -pt. is C/C/C
afebrile
PR- 101bpm
BP- 110/70mmhg
RR- 20cycles/min
spo2- 79% on ROOM AIR
90% ON NRBM at 15lt of oxygen
GRBS- 136mg/dl
CVS- s1s2 heard
R/S- BAE +
P/A- soft and non tender with no organomegaly
CNS- HMF intact
no pedal edema , jaundice .
investigation advised today is D-dimer and CRP
treatment being given:














Comments
Post a Comment